Hyponatremia nejm: Hyponatremia – PubMed
Severe Hyponatremia – Core EM
Definition: Hyponatremia is defined as any serum sodium < 135 mEq/L. Severe symptomatic hyponatremia typically occurs at a serum sodium < 120 mEq/L though the rapidity of the change in sodium is a key factor in the development of symptoms
Causes of Hyponatremia
- Hypervolemic Hyponatremia: Total body sodium increased with a relatively larger increase in total body water
- Chronic renal failure
- Cirrhosis
- Heart failure
- Euvolemic Hyponatremia: Total body sodium normal but increased total body water
- SIADH
- Drug related: Diuretics, opioids, barbiturates, carbamazepine
- Psychogenic polydipsia
- Hypothyroidism
- Adrenal insufficiency
- Water intoxication
- SIADH
- Hypovolemic Hyponatremia: Both total body sodium and water are decreased but sodium to a greater extent
- Fluid loss: vomiting, diarrhea, sweating, GI suction
- Renal causes: salt-wasting nephropathies, renal tubular acidosis, mineralocroticoid deficiency, diuretics, osmotic diuresis
- Third spacing fluids: burns, rhabdomyolysis, bowel obstruction
- Dilutional Hyponatremia: Hyperglycemia (i.
 e. in DKA, Hyperosmolar hyperglycemic states)
e. in DKA, Hyperosmolar hyperglycemic states) - Pseudohyponatremia: hyperlipidemia, hyperproteinemia
Clinical Manifestations
- The clinical manifestations define the severity of the hyponatremia (i.e. the serum level does not define severity). Symptoms and signs are dependent on both the serum level as well as the rapidity of change in the serum sodium
- Mild/moderate Hyponatremia
- Headache
- Nausea/vomiting
- Muscle cramps
- Lethargy
- Restlessness
- Severe Hyponatemia
- Disorientation
- Focal neurologic deficits
- Seizures (Status epilepticus common)
- Coma
Diagnosis
- There are no classic physical exam or EKG findings (unlike in other electrolyte abnormalities) to use to clinch the diagnosis
- Due to vagueness of symptoms in mild/moderate hyponatremia and the non-specific nature of symptoms in severe hyponatremia, the diagnosis may be suspected but will be confirmed by obtaining a serum sodium level
- ALL patients with altered mental status, seizures or neurologic deficits should have their serum sodium level assessed
Hyponatremia Algorithm (EM Cases)
Read More
EM Cases: Podcast 60: Emergency Management of Hyponatremia
Pfenning CL, Slovis CM: Electrolyte Disorders; in Marx JA, Hockberger RS, Walls RM, et al (eds): Rosen’s Emergency Medicine: Concepts and Clinical Practice, ed 8. St. Louis, Mosby, Inc., 2014, (Ch) 125: p 1636-53.
St. Louis, Mosby, Inc., 2014, (Ch) 125: p 1636-53.
References
Adrogue HJ, Maidas NE. Hyponatremia. NEJM 2000; 342(21): 1581-9. PMID: 10824078
Mohamand HK et al. Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol 2007; 2: 1110-7. PMID: 17913972
Moritz ML, Ayus JC. 100 cc 3% sodium chloride bolus: a novel treatment for hyponatremic encephalopathy. Metab Brain Dis 2010; 25: 91-6. PMID: 20221678
Sterns RH et al. Treating profound hyponatremia: a strategy for controlled correction. Am J Kidney Dis 2010; 56: 774-9. PMID: 20709440
Freely Filtered 004 Hypernatremia — NephJC
The Filtrate (minus Swapnil) gather to talk about the treatment of hypernatremia.
Joel Topf
Jennie Lin
Matt Sparks
Samira Farouk
The strange story of Jennifer Strange.
https://insiderexclusive.com/radios-deadly-stunts-the-jennifer-strange-story/
Water Poker
https://www.thelocal.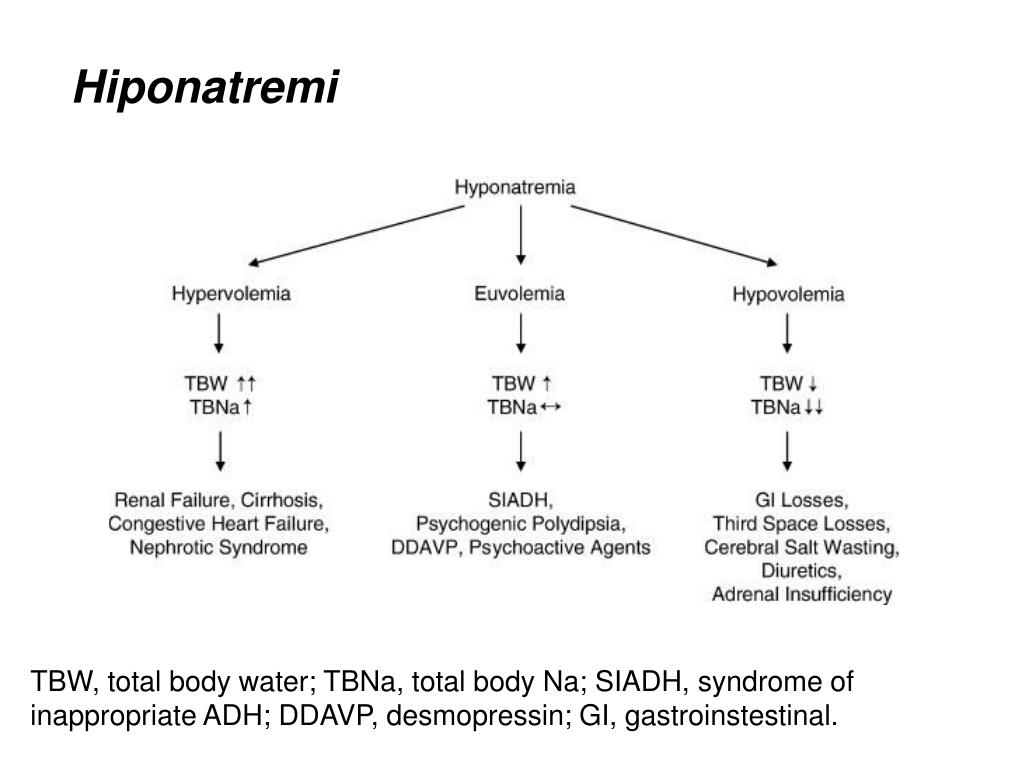 se/20120706/41878
se/20120706/41878
Nintendo Game Consoles
https://en.wikipedia.org/wiki/Nintendo_video_game_consoles
2019 Narins winner, Mitchel Rosner on MDMA induced hyponatremia
https://www.ncbi.nlm.nih.gov/pubmed/18684895
And Rosner again on exercise induced hyponatremia.
https://cjasn.asnjournals.org/content/2/1/151
The Arieff article on the dangers of severe hyponatremia: Hyponatremia, Convulsions, Respiratory Arrest, and Permanent Brain Damage after Elective Surgery in Healthy Women
https://www.nejm.org/doi/full/10.1056/NEJM198606123142401
The Richard Sterns article on the dangers of rapid correction of hyponatremia: Osmotic Demyelination Syndrome Following Correction of Hyponatremia
https://www.nejm.org/doi/10.1056/NEJM198606123142402
The editorial by the man himself, Robert Narins: Therapy of Hyponatremia
https://www.nejm.org/doi/full/10.1056/NEJM198606123142409
The infant study showing seizures associated with rapid correction of hypernatremia.
https://www.ncbi.nlm.nih.gov/pubmed/35558?dopt=Abstract
Follow up study with oral rehydration.
https://www.ncbi.nlm.nih.gov/pubmed/3958850?dopt=Abstract
The Linder study of adults admitted to the ICU
https://www.ncbi.nlm.nih.gov/pubmed/18037096
French study on patients presenting to the ER with hypernatremia.
https://bmcnephrol.biomedcentral.com/articles/10.1186/1471-2369-15-37
Study on US veterans showing poorer outcomes with slow correction of hypernatremia.
https://www.ncbi.nlm.nih.gov/pubmed/21358313
Cerebral edema during the treatment of DKA.
https://emj.bmj.com/content/21/2/141
The MIMIC 3 Database. MIMIC is an openly available dataset developed by the MIT Lab for Computational Physiology, comprising deidentified health data associated with ~40,000 critical care patients. It includes demographics, vital signs, laboratory tests, medications, and more.
https://mimic.physionet.org
Chalrson Comorbidity Index
https://www.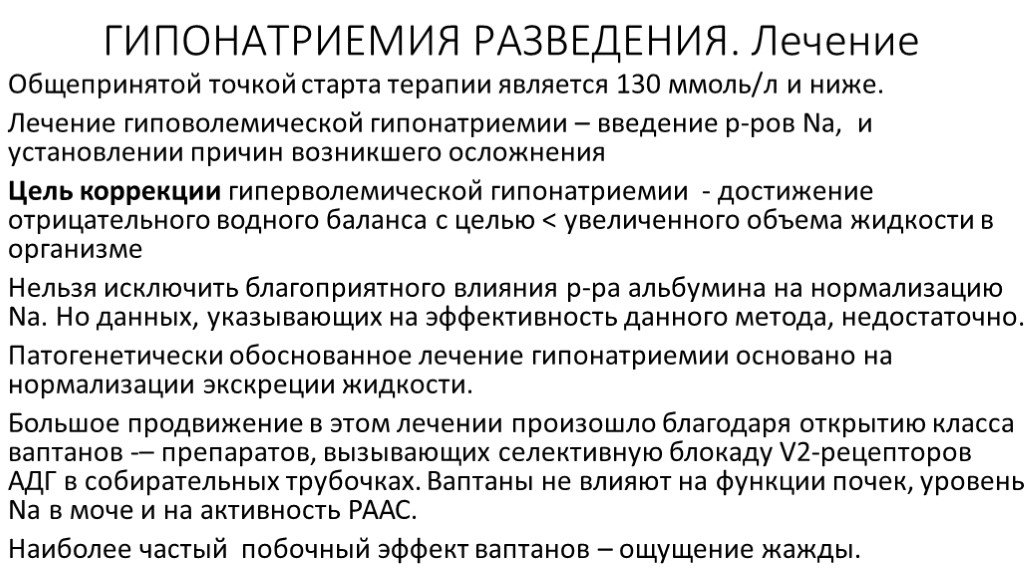 mdcalc.com/charlson-comorbidity-index-cci#creator-insights
mdcalc.com/charlson-comorbidity-index-cci#creator-insights
The paper: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation.
https://www.ncbi.nlm.nih.gov/pubmed/3558716
JCI article on organic brain osmnoles in response to hypernatremia
https://www.ncbi.nlm.nih.gov/pubmed/2332498?dopt=Abstract
John Booth on the value of MIMIC 3
phenomenal resource! Huge, and publicly available dataset, just waiting to be interrogate with juicy questions such as @scoc1 's … #nephJC
— John Booth (@ThePeanutKidney) May 15, 2019
Sri Lekha on checking labs in hypernatremia
I think primary teams perceive that nephrologists want to check labs frequently. Great to show that's not the case. We want to check when indicated. #nephjc
— Sri Lekha Tummalapalli, MD, MBA (@LTummalapalli) May 15, 2019
Steve Coca on chunky water administration
As I posted before, if this study prevents the incessant checking of S[Na] driving the patient and doctors nuts with the sticks and repeating strings of S[Na], then I will be happy.
Just set it and forget it. Give a nice chunky rate of water and come back tomorrow. #NephJC
— Steven Coca (@scoca1) May 15, 2019
Steve Coca musing the Cersei’s sodium level
Hmmmm….well there was Cersei sucking the water off the ground when she was imprisoned. Was she hypernatremic? #NephJC
— Steven Coca (@scoca1) May 15, 2019
Steve Coca swearing in High Valarlian:
https://twitter.com/scoca1/status/1128629713826721792
Steve Coca proving the non-existence of hypernatremia therapy being associated with brain damage through the inability of trial lawyers to find and sue doctors for this issue:
https://twitter. com/scoca1/status/1128652586612080642
com/scoca1/status/1128652586612080642
The original paper on the Kardashian Index
https://genomebiology.biomedcentral.com/articles/10.1186/s13059-014-0424-0
Kardashian Index Calculator
Facebook CEO Mark Zuckerberg says the ‘future is private’
https://www.theverge.com/2019/4/30/18524188/facebook-f8-keynote-mark-zuckerberg-privacy-future-2019
Khenar Jhaveri et al on ‘WhatsApp’ening in nephrology training
https://academic.oup.com/ckj/advance-article/doi/10.1093/ckj/sfz045/5482109
Mike Morrison’s video on how to rebuild the scientific poster
Mike’s Twitter: https://twitter.com/mikemorrison?lang=en with lot’s of examples of his design in the wild.
Make your own QR code: https://www.qr-code-generator.com
GoodRx: https://www.goodrx.com
Ten Worst Drugs for your Kidney: https://www.goodrx.com/blog/10-worst-medications-for-your-kidneys/
Drugs that can falsely elevate your creatinine levels: https://www. goodrx.com/blog/drugs-cause-false-high-creatinine-levels-blood-test/
goodrx.com/blog/drugs-cause-false-high-creatinine-levels-blood-test/
Dr Orrange, not wishing to engage on Twitter in a meaningful way: https://twitter.com/Orrangemd/status/1129165083194511361
Hyponatremia, what kind of disease, symptoms, diagnosis, treatment
Adamant
medical clinic
St. Petersburg, embankment of the river Moika, 78.
+7 (812) 740-20-90
Content:
Hyponatremia – fluid retention in the body, which leads to a sharp decrease in the amount of sodium in the blood to a critical level – below 135 mmol / l. The disease is extremely dangerous due to its unpredictability and swiftness. Its most severe complication is cerebral edema. Several causes can cause hyponatremia. That is why the doctors of Adamant Medical Clinic will conduct a comprehensive analysis of your body. This will allow you to diagnose the cause of the disease with high accuracy and immediately begin treatment.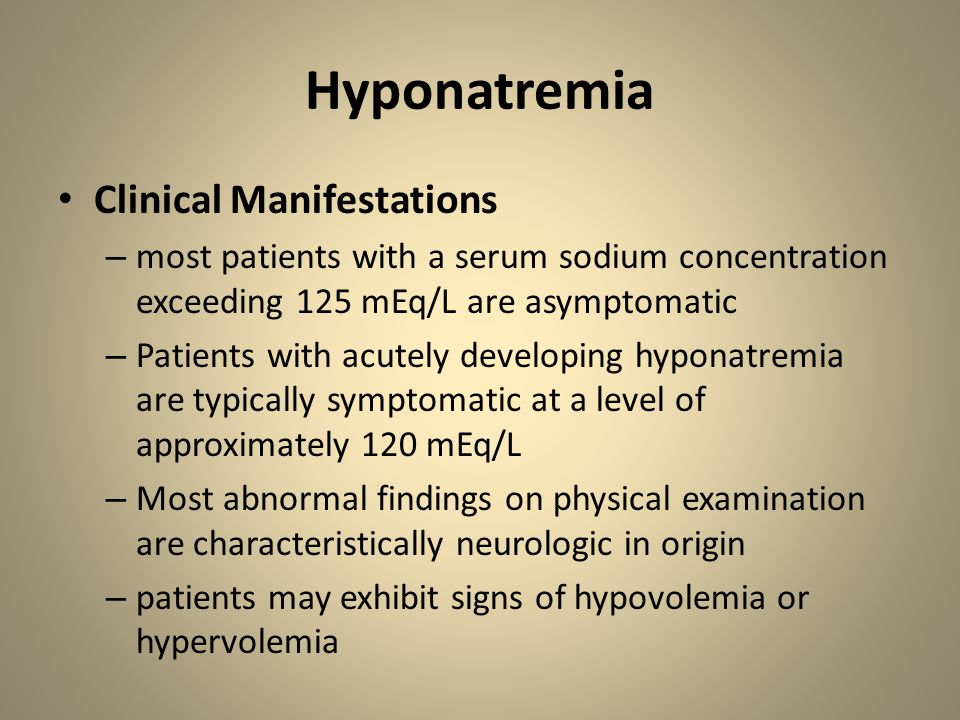 nine0004
nine0004
Symptoms of hyponatremia
The severity of symptoms of hyponatremia depends on the rapidity of the disease. If the disease progresses slowly, then it is almost asymptomatic. Its signs appear after a long time, when the concentration of sodium in the blood drops to a critical level. With the rapid development of hyponatremia, deterioration occurs within two days.
It causes swelling of the brain, which has the following symptoms:
- drowsiness;
- nausea and vomiting;
- confusion;
- impaired coordination of movements;
- convulsions.
Lack of urgent medical attention for hyponatremia will lead to coma. In the most severe cases, death. In order to avoid dangerous consequences at the first symptoms of hyponatremia, contact Adamant Medical Clinic! Our specialists will arrive at the address you specified as soon as possible and will provide all the necessary assistance, which will allow you to save your life and health! nine0004
Causes of hyponatremia
Low blood sodium in hyponatremia due to retention of excess water in the body is the main cause of the disease. This state is called:
This state is called:
Extrarenal losses:
- diarrhea and vomiting;
- burns, peritonitis, pancreatitis.
Kidney loss:
nine0023
- lack of mineralocorticoids;
- the use of diuretics;
- salt-losing nephropathy;
- osmotic diuresis.
Non-renal disorders:
- heart failure;
- cirrhosis;
- nephrotic syndrome.
nine0078
As you can see, hyponatremia is a consequence of diseases that can be recognized in advance, without bringing your body to a critical state. In case of problems with your health, please contact Adamant Medical Clinic, our specialists will conduct a complete examination of your body and immediately begin treatment!
Hyponatremia: a clinical approach
AVP – arginine-vasopressin
MD – medicinal products
BMD – bone mineral density
SIADH – syndrome of inappropriate secretion of antidiuretic hormone
STN – salt-losing nephropathy
CHF – chronic heart failure
CNS – central nervous system
CPU – cirrhosis of the liver
Abstract
Hyponatremia, defined as a decrease in serum sodium to 135 mmol/l or less, is the most common electrolyte disorder. The development of hyponatremia indicates a relative increase in the content of osmotically unbound water compared to the content of sodium in the body. This imbalance is a consequence of the excess consumption of osmotically free water over the ability of the renal tubules to dilute urine. In most cases, excess free water in the body is caused by increased secretion of the antidiuretic hormone, arginine-vasopressin (AVP), under the influence of osmotic and non-osmotic stimuli [1]. nine0004
The development of hyponatremia indicates a relative increase in the content of osmotically unbound water compared to the content of sodium in the body. This imbalance is a consequence of the excess consumption of osmotically free water over the ability of the renal tubules to dilute urine. In most cases, excess free water in the body is caused by increased secretion of the antidiuretic hormone, arginine-vasopressin (AVP), under the influence of osmotic and non-osmotic stimuli [1]. nine0004
AVP is synthesized in the neurosecretory cells of the supraoptic and paraventricular nuclei of the hypothalamus, accumulates in the posterior pituitary gland and is released in response to an increase in blood plasma osmolarity. Even a small increase in plasma osmolarity (by 1%) causes the secretion of the hormone. AVP secretion is also regulated by non-osmotic stimuli. The concentration of AVP in the blood increases with a decrease in mean arterial pressure by 5–7% or a decrease in the effective volume of arterial circulation (“underfilling of the arterial bed”) by 8–10% [1, 2]. nine0004
nine0004
The effects of AVP are mediated by vasopressin receptors V1a, V1b and V2. Activation of V1a receptors in the vascular wall leads to systemic vasoconstriction. V1b receptors are predominantly located in the anterior pituitary gland. V2 receptors are localized mostly in the collecting ducts of the kidneys. When they are activated, a type 2 aquaporin free water channel protein moves to the apical surface of the latter, which increases the reabsorption of osmotically free water [3, 4].
nine0005 The prevalence of hyponatremia in general therapeutic outpatient practice is not exactly known and, according to various sources, ranges from 21 to 34% [5-6]. In the elderly and in critically ill patients, the prevalence of hyponatremia is higher due to impaired urine dilution function and the ability to excrete osmotically free water.
Acute hyponatremia and, accordingly, a sharp decrease in extracellular osmolarity lead to an increase in intracranial pressure and the development of cerebral edema [7]. In the clinic of internal diseases, the so-called acute hyponatremic encephalopathy is an emergency situation, accompanied by high mortality (up to 42%). Concomitant hypoxia worsens the prognosis even more [8]. Chronic asymptomatic hyponatremia is also associated with a poor prognosis in hospitalized patients, including an increase in mortality and an increase in the length of stay in the hospital. At the same time, the prognosis is equally unfavorable, regardless of whether the patient arrives with hyponatremia or the latter develops during the hospital stay [9, 10]. The prevalence of hyponatremia in various conditions is presented in the table.
In the clinic of internal diseases, the so-called acute hyponatremic encephalopathy is an emergency situation, accompanied by high mortality (up to 42%). Concomitant hypoxia worsens the prognosis even more [8]. Chronic asymptomatic hyponatremia is also associated with a poor prognosis in hospitalized patients, including an increase in mortality and an increase in the length of stay in the hospital. At the same time, the prognosis is equally unfavorable, regardless of whether the patient arrives with hyponatremia or the latter develops during the hospital stay [9, 10]. The prevalence of hyponatremia in various conditions is presented in the table.
Prevalence of hyponatremia [13] Note. CHF – chronic heart failure.
Hyponatremia in the syndrome of inappropriate secretion of antidiuretic hormone (SIADH). This is a clinical symptom complex in which excessive unregulated secretion of AVP leads to the development of hyponatremic overhydration. SIADH is the main cause of euvolemic hyponatremia – hyponatremia with normal volume of circulating blood, plasma and extracellular fluid. The diagnosis of SIADH requires the exclusion of hypervolemic hyponatremia in diseases accompanied by the development of edema (see below), and hypovolemic hyponatremia, which occurs with significant losses of water and sodium through the gastrointestinal tract (diarrhea, vomiting, loss to the “third space”) or kidneys (overdose diuretics, especially those acting distally, primary adrenal insufficiency, salt-losing nephropathy – STN, glucosuria in diabetes mellitus, bicarbonaturia with the development of metabolic alkalosis, salt-losing syndrome with damage to the central nervous system – CNS). Other causes of euvolemic hyponatremia are severe hypothyroidism and glucocorticoid deficiency in hypopituitarism. In these situations, hyponatremia is corrected by hormone replacement therapy [11, 12]. nine0004
The diagnosis of SIADH requires the exclusion of hypervolemic hyponatremia in diseases accompanied by the development of edema (see below), and hypovolemic hyponatremia, which occurs with significant losses of water and sodium through the gastrointestinal tract (diarrhea, vomiting, loss to the “third space”) or kidneys (overdose diuretics, especially those acting distally, primary adrenal insufficiency, salt-losing nephropathy – STN, glucosuria in diabetes mellitus, bicarbonaturia with the development of metabolic alkalosis, salt-losing syndrome with damage to the central nervous system – CNS). Other causes of euvolemic hyponatremia are severe hypothyroidism and glucocorticoid deficiency in hypopituitarism. In these situations, hyponatremia is corrected by hormone replacement therapy [11, 12]. nine0004
It is necessary to note the possibility of developing hyponatremia with suppressed AVP synthesis in the case of drinking a very large amount of liquid with limited salt intake (true water intoxication).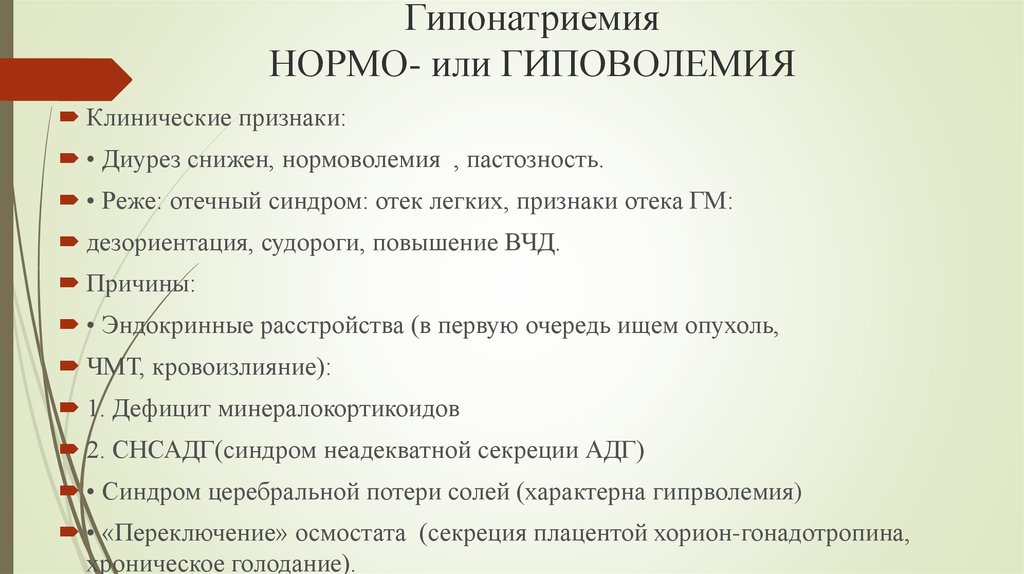 With a daily osmotic load of 600 mOsm or more and suppressed AVP synthesis (normal state), electrolyte balance can be maintained at standard values when drinking up to 12 liters of liquid. Thus, in patients with primary psychogenic polydipsia, hyponatremia develops with the use of more than 12 liters of fluid per day. Limiting the osmotic load to 300 mOsm in the absence of APV secretion leads to the development of hyponatremia when 6 liters are consumed. This is how “beer sweating” develops, when, with a very large amount of beer drunk (hypoosmolar fluid) and insufficient intake of salts, hyponatremia occurs, despite the almost complete suppression of AVP synthesis and the maximum ability of the kidneys to dilute. nine0004
With a daily osmotic load of 600 mOsm or more and suppressed AVP synthesis (normal state), electrolyte balance can be maintained at standard values when drinking up to 12 liters of liquid. Thus, in patients with primary psychogenic polydipsia, hyponatremia develops with the use of more than 12 liters of fluid per day. Limiting the osmotic load to 300 mOsm in the absence of APV secretion leads to the development of hyponatremia when 6 liters are consumed. This is how “beer sweating” develops, when, with a very large amount of beer drunk (hypoosmolar fluid) and insufficient intake of salts, hyponatremia occurs, despite the almost complete suppression of AVP synthesis and the maximum ability of the kidneys to dilute. nine0004
In patients with SIADH, hyponatremia develops with plasma hypoosmolarity and sufficient urine osmolality (more than 100 mOsm per 1 kg of water). In 10% of patients with hyponatremia and SIADH, diagnosed according to generally accepted criteria, the level of AVP in the blood cannot be determined. Probably, in these cases, the hormone is released at concentrations below the threshold of existing identification methods. Another explanation could be the development of nephrogenic SIADH in these patients associated with a mutation in the V2 receptor gene [13, 14]. nine0004
Probably, in these cases, the hormone is released at concentrations below the threshold of existing identification methods. Another explanation could be the development of nephrogenic SIADH in these patients associated with a mutation in the V2 receptor gene [13, 14]. nine0004
The etiology of SIADH is diverse and includes a number of tumors, diseases of the central nervous system, lungs, the influence of drugs (LP), etc. The second most common cause of SIADH after tumors are diseases of the central nervous system. Any diffuse brain injury, including trauma, can lead to SIADH [15]. The latter can also develop with an exacerbation of almost any mental illness. At the same time, the nature of SIADH cannot be clarified in 40% of patients, especially the elderly [13].
nine0005 LP-induced hyponatremia. L.P. is a common cause of hyponatremia. Hypovolemic hyponatremia due to the use of diuretics with severe dehydration develops quite rarely. However, distally acting diuretics and spironolactone can lead to the development of euvolemic hyponatremia associated with a violation of the concentration function of the tubules. Thiazide diuretics are a common cause of hyponatremia due to their widespread use. Other L.P. causing hyponatremia are presented below [16]. nine0004
Thiazide diuretics are a common cause of hyponatremia due to their widespread use. Other L.P. causing hyponatremia are presented below [16]. nine0004
LP associated with hyponatremia (except thiazide diuretics):
AVP analogues: desmopressin, oxytocin.
Drugs that enhance the renal effect of AVP: chlorpropramide, cyclophosphamide, non-steroidal anti-inflammatory drugs, acetaminophen (paracetamol).
Drugs that increase the release of AVP in the pituitary gland: chlorpropamide, clofibrate, carbamazepine, vincristine, nicotine, opiates, ifosfamide; nine0004
Mechanism of hyponatremia unknown: haloperidol, fluphenazine, amitriptyline, thioridazine, fluoxetine, methamphetamine (ecstasy), sertraline.
Among them, the most common causes of hyponatremia are psychopharmacological drugs: carbamazepine, oxcarbamazepine and antidepressants from the group of selective serotonin reuptake inhibitors. Severe hyponatremia can develop with the use of drugs that act on the serotonin system (ecstasy, 3,4-methylenedioxymethamphetamine) [17]. nine0004
Severe hyponatremia can develop with the use of drugs that act on the serotonin system (ecstasy, 3,4-methylenedioxymethamphetamine) [17]. nine0004
Hyponatremia in cancer patients. About 14% of the causes of hyponatremia in hospitalized patients are malignant neoplasms [18]. In most cases, hyponatremia develops in patients with an established diagnosis of a tumor, but in some cases it precedes the detection of a neoplasm. In cancer patients, hyponatremia can complicate surgical or chemotherapy treatment, being an unfavorable prognostic factor in this category of patients [19].].
The main mechanism for the development of hyponatremia in malignant neoplasms is the ectopic production of AVP by the tumor, which leads to the development of SIADH. Most often, hyponatremia develops in lung cancer, especially small cell (in 10-15% of patients), as well as tumors of the head and neck. The latter are accompanied by the development of SIADH in about 3% of cases. At the same time, hyponatremia most often develops in patients with malignant neoplasms of the oral cavity, less often – of the pharynx, larynx, sinuses and salivary glands [20]. It is possible, however, the development of SIADH in tumors of other localizations. nine0004
It is possible, however, the development of SIADH in tumors of other localizations. nine0004
The development of hyponatremia in cancer patients may complicate treatment with chemotherapy drugs, including vincristine, vinblastine, and cyclophosphamide [21]. The use of cisplatin and preparations based on it can lead to the development of STN, hypovolemia, and hypovolemic hyponatremia [22].
The use of large volume wound irrigation solutions for transurethral resection of the prostate or endometrial ablation can also cause transient hyponatremia [23]. nine0004
Hyponatremia in the elderly. The prevalence of hyponatremia increases with age, as evidenced by its prevalence in patients in nursing homes, which is 18-22.5% [24, 25]. Most of these patients had at least one cause of hyponatremia, but in 7% of cases no clear cause could be identified. It should be noted that in the group of patients older than 75 years, hyponatremia was detected in 43% of cases, and all of them met the criteria for SIADH [24]./44-1.jpg) nine0004
nine0004
The true cause of hyponatremia in the elderly is unclear, but there are several hypotheses that explain this condition. It is likely that with age, a violation of sodium metabolism develops, close to SIADH [24]. Elderly patients have mild hyponatremia at baseline, but comorbidities or LP may exacerbate this, resulting in neurological symptoms. A certain contribution to the development of hyponatremia in patients of this category is also made by a decreasing feeling of thirst, which leads to hypovolemic hyponatremia [26]. nine0004
Hyponatremia and fractures: imbalance and progression of osteoporosis. Chronic hyponatremia leads to the development of cognitive impairment, balance disorders and associated falls. In the presence of asymptomatic hyponatremia, the frequency of falls increases to 21.3% versus 5.4% in patients of the same age, but without impaired sodium metabolism [25].
The relationship between hyponatremia and decreased bone mineral density (BMD) has been studied in a number of studies.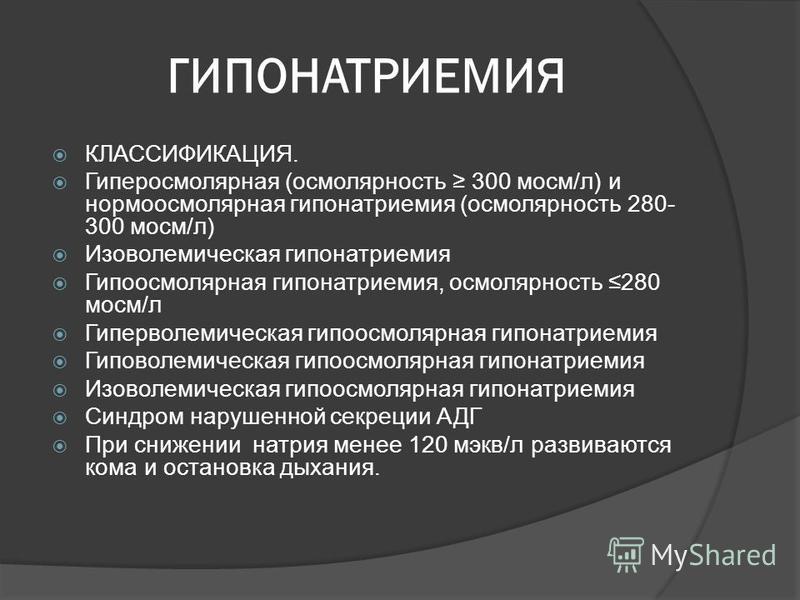 It is known that bones contain about 1/3 of all sodium reserves, and 40% of this sodium is able to enter the blood. In animal experiments, a decrease in BMD by 30% or more with prolonged hyponatremia has been demonstrated. It is likely that in chronic hyponatremia, sodium is activated from the bone tissue into the blood, which promotes the resorption of the bone matrix and bone demineralization [27]. Hyponatremia also increases the activity of osteoclasts, although the direct mechanism of this phenomenon is not well understood [28]. nine0004
It is known that bones contain about 1/3 of all sodium reserves, and 40% of this sodium is able to enter the blood. In animal experiments, a decrease in BMD by 30% or more with prolonged hyponatremia has been demonstrated. It is likely that in chronic hyponatremia, sodium is activated from the bone tissue into the blood, which promotes the resorption of the bone matrix and bone demineralization [27]. Hyponatremia also increases the activity of osteoclasts, although the direct mechanism of this phenomenon is not well understood [28]. nine0004
Hyponatremia with significant physical exertion. Hyponatremia can develop acutely during strenuous exercise, including marathon, ultramarathon, and triathlon participants [29]. The prevalence of hyponatremia among amateur marathon runners is 3–13% [30–32]. A correlation was shown between the incidence of hyponatremia and an increase in body weight during the race, probably due to the unlimited use of drinking water, which is a hypoosmolar solution. There are also data on non-osmotic secretion of AVP during intense long-term exercise [33]. Risk factors for the development of hyponatremia in marathon participants are female gender, body mass index less than 20 kg/m 2 and relatively low running speed in less trained athletes [30]. Acute severe hyponatremia can lead to severe neurological symptoms, including cerebral edema and seizures, neurogenic pulmonary edema, and even death.
There are also data on non-osmotic secretion of AVP during intense long-term exercise [33]. Risk factors for the development of hyponatremia in marathon participants are female gender, body mass index less than 20 kg/m 2 and relatively low running speed in less trained athletes [30]. Acute severe hyponatremia can lead to severe neurological symptoms, including cerebral edema and seizures, neurogenic pulmonary edema, and even death.
Hyponatremia in CHF. The hypervolemic variant of hyponatremia is mainly found in CHF and cirrhosis of the liver (LC). The incidence of hyponatremia in decompensated CHF, according to some data, reaches 38% [9, 34]. The association of hyponatremia with an increase in total and cardiovascular mortality, as well as with repeated hospitalizations and low quality of life in these patients, has been demonstrated. In patients with CHF, in addition, the presence of hyponatremia increases the length of stay in the hospital and the risk of developing acute cardiorenal syndrome, and the adverse prognostic effect of hyponatremia persists even with long-term follow-up (4–5 years) [35, 36].
In CHF, hyponatremia develops despite plasma hypoosmolarity, in which AVP synthesis is normally maximally suppressed. The cause of hyponatremia in CHF is the non-osmotic secretion of AVP. In CHF, with a decrease in cardiac output, the stretching of baroreceptors in the wall of the aortic arch and carotid sinus decreases, which leads to disruption of the normal tonic inhibitory effect of the CNS mediated by the vagus and glossopharyngeal nerves [37]. The result is an increase in efferent sympathetic activity, which causes stimulation of the renin-angiotensin-aldosterone system and non-osmotic release of AVP [38]. nine0004
The development of hyponatremia thus reflects an extremely dangerous combination of low cardiac output and maximum activation of neurohumoral systems, which is associated with a poor prognosis in many cardiac patients, including those with primary pulmonary hypertension, pulmonary embolism, and after cardiac surgery [39— 41].
Hyponatremia in cirrhosis. The main mechanism for the development of hyponatremia in cirrhosis is non-osmotic secretion of AVP, caused by “underfilling” of the arterial bed due to systemic (primarily intra-abdominal) vasodilation against the background of portal hypertension [42, 43]. Apparently, the main mechanism of vasodilation in cirrhosis is the effect of nitric oxide [44]. Hyponatremia in patients with cirrhosis is a predictor of hepatorenal syndrome and increases the risk of hepatic encephalopathy [45]. In a study of more than 500 patients with cirrhosis, hyponatremia was found to be a strong predictor of reduced quality of life and a worsening prognosis after liver transplantation [46–49].
The main mechanism for the development of hyponatremia in cirrhosis is non-osmotic secretion of AVP, caused by “underfilling” of the arterial bed due to systemic (primarily intra-abdominal) vasodilation against the background of portal hypertension [42, 43]. Apparently, the main mechanism of vasodilation in cirrhosis is the effect of nitric oxide [44]. Hyponatremia in patients with cirrhosis is a predictor of hepatorenal syndrome and increases the risk of hepatic encephalopathy [45]. In a study of more than 500 patients with cirrhosis, hyponatremia was found to be a strong predictor of reduced quality of life and a worsening prognosis after liver transplantation [46–49].
Clinical approach for hyponatremia. The diagnostic algorithm in the presence of hypotonic hyponatremia is shown in the figure [50]. The use of this algorithm requires the exclusion of isotonic hyponatremia resulting from paraproteinemias, massive infusion of gamma globulins, the use of radiopaque agents, and severe hyperlipidemia (especially hypertriglyceridemia).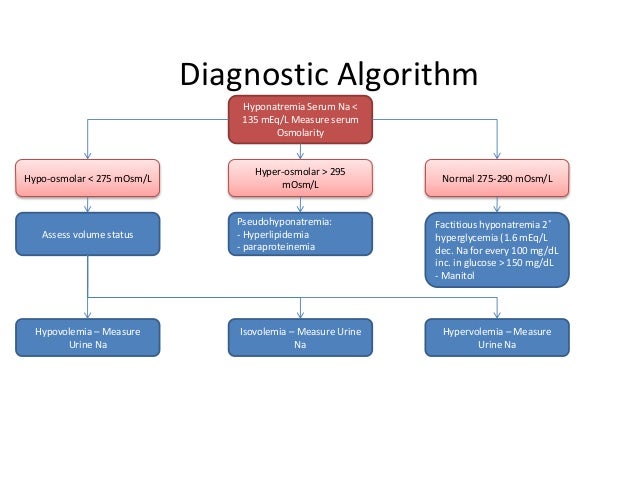 Hyperosmolar conditions (hyperglycemia, mannitol infusion, significant positive anion gap) must also be ruled out. Thus, in all cases of hyponatremia, it is desirable to preliminarily determine the plasma osmolarity. Urinary osmolality in patients with hyponatremia usually exceeds 100 mOsm/kg. However, in patients with primary polydipsia and salt restriction (eg, beer sweating), urine osmolality may be low. It should be noted that pronounced natriuresis when taking diuretics can make it difficult to interpret indicators of urinary sodium excretion. nine0004
Hyperosmolar conditions (hyperglycemia, mannitol infusion, significant positive anion gap) must also be ruled out. Thus, in all cases of hyponatremia, it is desirable to preliminarily determine the plasma osmolarity. Urinary osmolality in patients with hyponatremia usually exceeds 100 mOsm/kg. However, in patients with primary polydipsia and salt restriction (eg, beer sweating), urine osmolality may be low. It should be noted that pronounced natriuresis when taking diuretics can make it difficult to interpret indicators of urinary sodium excretion. nine0004
Clinical approach to the diagnosis and treatment of hyponatremia. AKI – acute renal failure; CRF – chronic renal failure.
The next step is to determine the total body fluid content. Diagnosis of hypervolemic hyponatremia is usually not very difficult due to the presence of signs of severe hypervolemia (edema, ascites) in severe CHF or cirrhosis. In clinical practice, infusion of saline (0.5–1 L for 12 h) helps to differentiate hypovolemic and euvolemic hyponatremia [51]. In SIADH, in most cases (especially with urine osmolality greater than 500 mOsm/kg), the injected sodium is rapidly excreted without changing the sodium content in the blood. At the same time, in hypovolemic hyponatremia, volume replacement normalizes sodium homeostasis in the blood. It should be emphasized that in euvolemic hyponatremia, in contrast to hypovolemic hyponatremia due to the absolute excess of osmotically free water, there are lower levels of uric acid, urea and creatinine in the blood. Moreover, the increase in uric acid excretion and decrease in its concentration in the blood in SIADH is not impaired even in the case of diuretics [52, 53]. nine0004
In SIADH, in most cases (especially with urine osmolality greater than 500 mOsm/kg), the injected sodium is rapidly excreted without changing the sodium content in the blood. At the same time, in hypovolemic hyponatremia, volume replacement normalizes sodium homeostasis in the blood. It should be emphasized that in euvolemic hyponatremia, in contrast to hypovolemic hyponatremia due to the absolute excess of osmotically free water, there are lower levels of uric acid, urea and creatinine in the blood. Moreover, the increase in uric acid excretion and decrease in its concentration in the blood in SIADH is not impaired even in the case of diuretics [52, 53]. nine0004
The most reliable way to diagnose SIADH could be the determination of AVP in the blood. However, the complexity and high cost of the technique make it of little use in everyday clinical practice. In recent years, it has become possible to determine the content of copeptin in the blood, a stable glycopeptide formed from the precursor of AVP during the synthesis of the hormone in an equimolar ratio. Thus, the level of copeptin can indirectly indicate the content of AVP and differentiate primary polydipsia from SIADH [54]. nine0004
Thus, the level of copeptin can indirectly indicate the content of AVP and differentiate primary polydipsia from SIADH [54]. nine0004
If euvolemic hyponatremia, i.e. SIADH, is identified, the cause must be determined. First of all, the influence of a number of drugs, hypothyroidism and adrenal insufficiency should be rejected. The next step is to exclude the most common tumors leading to SIADH using computed tomography of the chest and magnetic resonance imaging of the brain. In some cases, especially in elderly patients, the genesis of SIADH cannot be established.
Therapy of hyponatremia. Management of hyponatremia depends on the type (hypovolemic, hypervolemic, or euvolemic), duration, and severity of symptoms. Regardless of the cause of hyponatremia, severe neurological symptoms (convulsions, coma, respiratory arrest) require the immediate administration of 3% hypertonic sodium chloride solution to reduce the severity of cerebral edema. It is recommended to administer 100 ml of the solution as a bolus, if necessary, the administration can be repeated after 30 minutes [55]. Thus, the sodium content in the blood increases by 2-4 mmol/l. In rare cases, 200 ml of hypertonic saline is insufficient to achieve a clinical effect. The effect of hypertonic saline may enhance the simultaneous administration of furosemide. Successful use of 30-60 ml of 23.4% hypertonic sodium chloride solution for herniation of the brain stem caused by hyponatremia is described. Such a solution makes it possible to increase the level of sodium in the blood by more than 5 mmol/l [56]. nine0004
Thus, the sodium content in the blood increases by 2-4 mmol/l. In rare cases, 200 ml of hypertonic saline is insufficient to achieve a clinical effect. The effect of hypertonic saline may enhance the simultaneous administration of furosemide. Successful use of 30-60 ml of 23.4% hypertonic sodium chloride solution for herniation of the brain stem caused by hyponatremia is described. Such a solution makes it possible to increase the level of sodium in the blood by more than 5 mmol/l [56]. nine0004
Hypertonic sodium chloride solution must be prepared in a pharmacy and is rarely available. An 8.4% sodium bicarbonate solution can be used as a means for an emergency increase in the level of sodium in the blood. The osmolarity of 8.4% sodium bicarbonate solution is 2000 mOsm/l, which corresponds to the osmolarity of 5.8% sodium chloride solution. Thus, 50 ml of 8.4% sodium bicarbonate solution is equivalent to 100 ml of 3% sodium chloride solution in terms of increasing blood sodium levels. nine0004
nine0004
With a rapid (within 24-48 hours), a significant decrease in the level of sodium in the blood, severe neurological symptoms develop. With a slower development of hyponatremia, “small” cerebral symptoms are noted: lethargy, disorientation, nausea, and impaired cognitive functions. In these cases, rapid progression to life-threatening conditions is possible, which also requires the use of hypertonic saline. At the same time, too rapid correction of hyponatremia is no less dangerous. Acute development of severe hyponatremia can lead to cerebral edema, however, with a longer exposure to electrolyte disorders (more than 48-72 hours), tissue adaptation occurs due to the diffusion of potassium and organic high-osmolar compounds (myrinositol, phosphocreatine) and amino acids (glutamine, taurine) from cells. In the latter case, a rapid increase in the level of sodium in the blood (more than 10–12 mmol/l/day) can lead to the development of a fatal complication of hypercorrection of hyponatremia — osmotic demyelination of the brain, which develops when the initial sodium level is less than 115–120 mmol/l [57, 58]. Risk factors for its development are concomitant severe liver disease, hypoxia, hypokalemia, cachexia, as well as an increase in the level of sodium in the blood of more than 25 mmol / l in 48 hours. Thus, the rate of correction of severe symptomatic hyponatremia should not exceed 10-12 mmol / l / days, and in patients with risk factors for the development of demyelination, chronic alcoholism and with an initial blood sodium level of less than 105 mmol/l – no more than 8 mmol/l/day [59].
Risk factors for its development are concomitant severe liver disease, hypoxia, hypokalemia, cachexia, as well as an increase in the level of sodium in the blood of more than 25 mmol / l in 48 hours. Thus, the rate of correction of severe symptomatic hyponatremia should not exceed 10-12 mmol / l / days, and in patients with risk factors for the development of demyelination, chronic alcoholism and with an initial blood sodium level of less than 105 mmol/l – no more than 8 mmol/l/day [59].
Minimal neurological symptoms in hyponatremia: headache, decreased concentration, irritability, decreased mood and depression usually develop in patients with chronic electrolyte disturbances. In this situation, in addition to the treatment of the underlying disease, it is sufficient to limit fluid intake (with eu- and hypervolemic variant). The degree of restriction depends on diuresis. So, with a daily diuresis of 1200 ml, the daily fluid intake should not exceed 750 ml. With this restriction of fluid, an increase in the level of sodium in the blood by 1-2 mmol / l per day is noted. The effectiveness of fluid restriction is reduced with a higher ratio of urine osmolarity to plasma osmolarity [59].
The effectiveness of fluid restriction is reduced with a higher ratio of urine osmolarity to plasma osmolarity [59].
In hypervolemic variants of hyponatremia (CHF and cirrhosis), the basis of therapy is the use of large doses of loop diuretics with correction of hypokalemia and hypomagnesemia. The development of hyponatremia in these diseases reflects a decrease in “effective arterial blood flow”, severe disorders of central hemodynamics, and activation of neurohumoral systems. With decompensated CHF, the development of hyponatremia may be another reason for transferring the patient to the intensive care unit and prescribing intravenous inotropic drugs or vasodilators. With C.P. due to the increased risk of developing hepatorenal syndrome, the development of hyponatremia necessitates the infusion of albumin and colloids, the appointment of vasopressors in appropriate cases, as well as dose adjustment of lactulose, since the osmotic effect of the drug can reduce the amount of osmotically free fluid in the body and increase the level of sodium in the blood. nine0004
nine0004
In order to correct hyponatremia, in addition to limiting fluid intake and using hypertonic solutions, in cases of developing CNS damage, it is possible to use demeclocycline, fludrocortisone, urea, as well as selective AVP receptor inhibitors, vaptans. Demeclocycline causes transient nephrogenic diabetes insipidus resistant to vasopressin, but the high toxicity of the drug limits its use in wide clinical practice [60].
Fludrocortisone is a mineralocorticoid hormone that enhances sodium absorption in the renal tubules. The use of this drug at a dose of 0.1-0.4 mg / day is the basis for the treatment of hyponatremia in adrenal insufficiency, as well as in salt-wasting syndrome with the development of hypovolemic hyponatremia, complicating brain damage. Successful use of the drug in SIADH against the background of small cell lung cancer has been described [61]. nine0004
Osmotic diuresis with increased excretion of osmotically unbound water and, accordingly, correction of hyponatremia can be induced with the use of urea (15-30 g / day in divided doses). Successful use of urea through a nasogastric tube (0.5–1 g/kg/day) has been described in the intensive care unit [62]. A similar efficacy of urea and vasopressin receptor antagonists (vaptans) was shown during long-term use in patients with hyponatremia of various origins [63]. Another approach to the treatment of hyponatremia is to prescribe loop diuretics for increased salt intake. nine0004
Successful use of urea through a nasogastric tube (0.5–1 g/kg/day) has been described in the intensive care unit [62]. A similar efficacy of urea and vasopressin receptor antagonists (vaptans) was shown during long-term use in patients with hyponatremia of various origins [63]. Another approach to the treatment of hyponatremia is to prescribe loop diuretics for increased salt intake. nine0004
Since most cases of hyponatremia are associated with the effect of AVP, blockade of its receptors by specific antagonists (vaptans) leads to the correction of electrolyte disturbances. The first drug from this group to find clinical use is conivaptan, a parenteral V1 and V2 receptor blocker [64]. The first oral V2 receptor blocker is tolvaptan. Long-term use (up to 3 years) of tolvaptan has been shown to be effective and safe; however, the first doses should be administered in a hospital setting to prevent too rapid an increase in sodium levels in the blood [65]. nine0004
Hyponatremia is a frequent violation of electrolyte metabolism in the clinical practice of internists, nephrologists, oncologists, cardiologists, hepatologists, neurologists and resuscitators. Hyponatremia can accompany many diseases and is associated with their poor prognosis. At the same time, severe hyponatremia, regardless of the cause, can pose a threat to the patient’s life. Much less is known about the significance of chronic mild hyponatremia.
Hyponatremia can accompany many diseases and is associated with their poor prognosis. At the same time, severe hyponatremia, regardless of the cause, can pose a threat to the patient’s life. Much less is known about the significance of chronic mild hyponatremia.
Approaches to the treatment of hyponatremia depend on the severity of neurological symptoms, its duration and type (hypo-, eu- or hypervolemic hyponatremia). In most cases (with the exception of the hypovolemic variant), hyponatremia reflects an excess of free water, and not a lack of sodium in the patient’s body as a result of a violation of the osmotic control system and osmotically independent secretion of ADH. The introduction of hypertonic sodium solution allows you to quickly eliminate the severe neurological manifestations of this electrolyte disorder. However, with long-term hyponatremia, therapeutic measures are aimed at suppressing the osmotically independent secretion of ADH or blocking the effect of ADH.